The Plain Truth About Face Masks

People have been using masks for a long time. The oldest masks ever found were 9,000 years old. Masks have been used for religious rituals, for fun, in factories to protect against breathing in chemicals and dust particles, for protection against smog, to punish slaves and gossipy wives, to commit crimes, and, of course, for Halloween. But the focus of this article will be about the medical use of masks.
Bubonic plague recurred in Europe for centuries. In 17th Century Europe, doctors who tended plague victims believed that it spread through poisoned air known as miasma that could create an imbalance in a person’s bodily fluids or humors. To protect themselves, physicians wore a long coat covered in scented wax, a hat and gloves made of goat leather, and a mask with a 6” long bird-like beak filled with herbs, cinnamon, myrrh, and perfume among other things. They also carried a long rod to poke or fend off victims with. Of course, all these silly outfits did was make them look ridiculous.
Image on the right: Carl Flugge
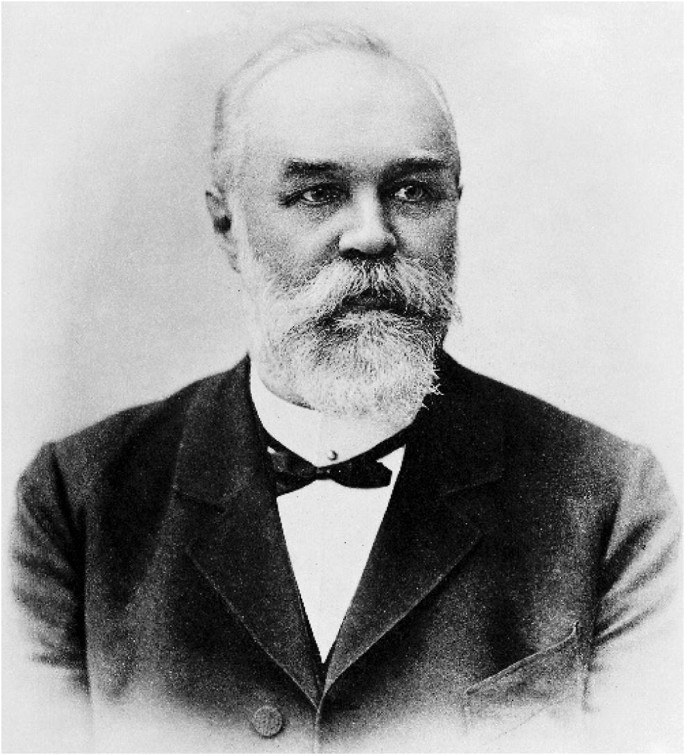
The first doctors to wear a mask in an operating room were Polish surgeon Johann Von Mikulicz Radecki and French surgeon Paul Berger in 1897. They advocated using masks during surgery due to the findings of German bacteriologist Carl Flugge who discovered pathogenic bacteria in saliva. Back then, surgical masks were made of several layers of gauze. The purpose of the surgical mask was, and still is, to prevent respiratory droplets from the physician’s nose and mouth from entering a patient’s open wound, and to protect the surgeon from sprays and splashes from the patient during an operation. But most doctors refused to go along with Radecki and Berger so it took many years after that before surgical masks became standard operating room equipment.
The first physician to have the lay public wear gauze masks was Chinese Doctor Wu Lein Teh during the Manchurian plague of 1910-1911 which killed around 63,000. This paved the way for some cities in our country to force the general public to wear masks during the 1918 influenza pandemic. It became known as the Spanish flu because the first cases were reported in Spain. But it may not have originated there. Due to WWI, news reporting in many countries was disrupted unlike Spain which had remained neutral. The Spanish flu killed between 50-100 million worldwide out of a back then global population of 1.8 billion.
Time Magazine ran a May 1, 2020 article hinting that forcing people to wear masks helped save lives during the 1918 influenza pandemic. Some mask advocates on social media sites like Facebook dogmatically make that claim. The scientific literature disagrees.
A May 12, 2020 article published in the peer review journal Health Affairs emphatically states: “Experts reviewing the evidence from 1918 concluded that flu masks failed to control infection.” The article goes on to cite a 1919 study by Wilfred H. Kellogg for the California State Board of Health: “…mask ordinances applied forcibly to entire communities did not decrease cases and deaths, as confirmed by comparisons of cities with widely divergent policies on masking.” Kellogg concluded: “The case against the mask as a measure of compulsory application for the control of epidemics appears to be complete.” Two other studies cited in the article, one from 1918 and another from 1921, reached the same conclusion.
Before we get into what modern science has to say about masks, it’s important to understand what isn’t science. Authoritative statements made by people with M.D. or PhD after their names is not science–the same goes for celebrities and billionaires. Decrees, directives, and executive orders made by politicians, corporate CEOs, directors of institutions, and public health authorities is not science. They may or may not be telling the truth. You have to check their sources and see if they represent any special interests that could create bias. To blindly believe them because they are so-called experts is to commit the appeal to authority fallacy. A logical fallacy is a mistaken belief based on unsound reasoning.
There are two kinds of scientific research. Observational and experimental. Statistical correlations and computer modeling (epidemiological studies) are examples of observational science. They can be useful in pointing the way to what needs to be looked at more closely and for quality control regarding treatments in clinical practice. These kind of studies can often wind up being very inaccurate if used by themselves.
The gold standard in science are randomized controlled trials with verified outcomes because they eliminate bias and speculation. For example, hormone replacement therapy. Originally, estrogen therapy was thought to reduce heart attacks. This was based on an observational study. But when a randomized controlled trial or experimental study was done it showed that estrogen therapy actually increased the risk of a heart attack. To make it simple, compare what I just said with going on a trip. Epidemiological and other observational studies are the travel route, randomized controlled trials with verified outcomes are the destination.
In the case of masks, some observational/epidemiological studies show that they lowered COVID-19 cases and death rates in places that mandate mask wearing as opposed to places that don’t. But there are also studies that show the opposite. For example, Michigan, population 10,045,000, very punitive lockdown restrictions, strict mask mandates. Sweden, population 10,110,405, no punitive lockdown restrictions, no mask mandates. Total COVID-19 deaths in Michigan: 7,019. Total COVID-19 deaths in Sweden: 5,880. One can cherry-pick this kind of data adnauseam, but it’s all speculation. The bottom line question is: do masks block viral particles? Only experimental studies or randomized controlled trials with verified outcomes can answer this question by testing the masks directly. Such studies have been done numerous times.
Source: Fast Company
Of the most comprehensive studies on masks was done in the United Kingdom in 2008 by the HSE (Health Safety Executive), it’s like our OSHA, entitled: “Evaluating the protection afforded by surgical masks against influenza bioaerosols” “Gross protection of surgical masks compared to filtering facepiece respirators” (N95 masks).
Background: “There is a common misconception amongst workers and employers that surgical masks will protect against aerosols…However, surgical masks are not intended to provide protection against infectious aerosols.”
Aerosols are very fine particles, much smaller than respiratory droplets, that are suspended in the fluid air for long periods of time and can travel quite far. We release these aerosols through breathing and speaking—they can contain large amounts of pathogenic viruses—the part of our body most vulnerable to them is the respiratory system.
In the HSE study, different kinds of masks were tested on a dummy’s head which was exposed to aerosols containing influenza virus particles to see if the masks would filter them out. Influenza virus is supposed to be similar in size to SARS-CoV-2, the virus that supposedly causes COVID-19.
Page 21: “Live infectious virus was extracted in enumerable quantities from the air from behind all the surgical masks tested. This suggests that influenza virus can survive in aerosol particles and bypass/penetrate a surgical mask and that a residual infectious aerosol hazard may exist.”
Page 22: “Even if the mask is manufactured from high efficiency filtering media, a high proportion of particles challenging the surgical mask will enter the breathing zone via breaches in the face seal. Furthermore, a high efficiency filtration media and fluid-resistant layers are likely to increase breathing resistance. This, together with a poor face fit, will increase the degree of leakage around the face seal.”
Page 23: “As surgical masks cannot be fitted well to the face, their use may not be adequate for protection against a residual airborne infection hazard.”
A June 26, 2019 study in Peer J—Journal of Life and Environmental Sciences: “Optimal microscopic study of surface morphology and filtering efficiency of face masks” demonstrated that cloth masks are even worse than surgical masks.
Background: “Low-cost face masks made from different cloth materials are very common in developing countries. The cloth masks (CM) are usually double layered with stretchable ear loops. It is common practice to use such masks for months after multiple washing and drying cycles. If a CM is used for long time, the ear loops become stretched. The loop needs to be knotted to make the mask loop fit better on the face.”
Conclusions: “Filtering efficiency of CM for ambient PM (particulate matter) was poorer than in SM (surgical masks). The poor efficiency was due to the presence of larger sized pores. Our study also demonstrated that washing and drying cycle deteriorates the filtering efficiency due to change in pore shape and clearance. We also found that stretching of the CM surface alters the pore size and potentially decreases the filtering efficiency. The findings of this study suggest that CM are not effective, and that effectiveness deteriorates if used after washing and drying cycles and if used under stretched condition.” And what does the CDC recommend? Washing cloth masks.
Bottom line: all masks, doesn’t matter what kind, have a network of microscopic pores/holes in them. If they didn’t, you wouldn’t be able to breath at all. Unlike the 1911 Manchurian plague which was caused by a bacterial pathogen, respiratory diseases like the Spanish flu are caused by viruses. The average size of most bacteria is between 0.2 and 2.0 microns. Viruses are a lot smaller. SARS-CoV-2 is between 0.06 and 0.14 microns which makes it a lot smaller than the pores in any mask. N95 masks have the smallest pores at 0.3 microns. But viruses don’t travel through the air by themselves—they travel via droplets and aerosols which are larger than the virus, but still small enough to go through the pores in any mask. The larger the pores in the mask the more particles and droplets will get through.
A June 1, 2020 study from AAPS (Association of American Physicians and Surgeons) reported on the filter efficiency of cloth masks and scarves for microscopic particles ranging in size from 0.02 – 1.0 microns: “Cloth masks 10% to 30%,” “Scarves 10% to 20%.” “All of the cloth masks and materials had near zero efficiency at 0.3 um (microns), a particle size that easily penetrates into the lungs.” The study further reported on the efficiency of 44 surgical masks and N95 respirators for particles ranging in size from 0.08 to 0.22 microns: “N95 FFR filter efficiency was greater than 95%.” “Medical masks – 55% efficiency” “General masks – 38%.”
Two things to keep in mind: one virion (cell free virus particle) is enough to cause infection if it enters into a cell and multiplies. This debunks the assertion that masks are better than nothing because they block some viral particles. Additionally, the CDC does not recommend N95 masks be worn by the general public in order to reserve them for health care workers. In order to block at least 95% of infectious viral particles, N95 masks have to be properly fitted to a person’s face in a clinical setting. Instead, the CDC recommends that the general public wear cloth masks which at best filters out only 30% of viral particles. Now I ask you: is this really about public health? Simply stated: wearing any kind of mask to prevent viral diseases is a waste of time.
The most thorough and comprehensive kind of scientific study is a systematic review usually combined with meta-analysis. It sits at the very top of the “Evidence Pyramid.” To quote the North Central University Library in Minnesota: “A systematic review is a high-level overview of primary research on a particular research question that systematically identifies, selects, evaluates, and synthesizes all high quality research evidence relevant to that question in order to answer it. In other words, it provides an exhaustive summary of scholarly literature related to a particular research topic or question. A systematic review is often written by a panel of experts after reviewing all the information from both published and unpublished studies.”
Numerous systematic reviews have been done on masks. All of them came to the same conclusion. Here are two of them:
Peer-review journal: Influenza and Other Respiratory Viruses, 2011 study “The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence” They reviewed 17 studies (see Discussion) and concluded: “None of the studies we reviewed established a conclusive relationship between mask/respirator use and protection against influenza infection.” The authors go on to say: “In conclusion, there is a limited evidence base to support the use of masks and/or respirators in healthcare or community settings.”
Probably the most comprehensive study ever done was by the peer-review journal Canadian Family Physician (CFP) in July 2020: “Masks for prevention of viral respiratory infections among health care workers and the public” “PEER umbrella systematic review” This study included 11 systematic reviews and 18 randomized controlled trials (RCTs) of 26,444 participants. The result:
Synthesis: “Overall, the use of masks in the community did not reduce the risk of influenza, confirmed viral respiratory infection, influenzalike illness, or any clinical respiratory infection.”
Community setting:“The use of masks in community settings in general did not reduce the risk of confirmed influenza…or confirmed viral respiratory infection. Results were not statistically significant in any subgroup analysis (masks worn by all, just the sick person, or just the healthy family members at home).”
Health care setting: “Of the 6 RCTs examining the use of masks by health care workers, only two had a control group assigned to no mask. In these trials, masks did not reduce influenzalike illness…any clinical respiratory infection…or confirmed viral respiratory infection compared with no masks.”
Discussion: “Particularly in the community setting, we wanted to see if there was any evidence of benefit from systematic use of masks by the general public outside the home, but we found no such evidence.”
There you have it. The latest most up to date body of knowledge on masks. Dr. Denis Rancourt, PhD summed it up best In his April 2020 paper “Masks Don’t Work” “A review of science relevant to COVID-19 social policy” published in Research Gate. Page 4: “No RCT study with verified outcome shows a benefit for HCW” (health care workers) “or community members in households to wearing a mask or respirator. There is no such study. There are no exceptions.”
Nevertheless, politicians, public health authorities, and the media continue to drone on about a growing body of evidence showing that masks worn by the general public are effective. In its June 5
“Interim Guidance” on masks, the WHO (World Health Organization) admits on page 6 that mask use by the general public “is not yet supported by high quality or direct scientific evidence…” Instead, they assert that “a growing compendium of observational evidence” indicates their possible effectiveness.
A July 31 article in the Journal of the American Medical Association (JAMA) warned that “observational studies” might “reduce the likelihood of a properly designed trial being performed, thereby delaying the discovery of reliable truth…if leaders, commentators, academics, and clinicians cannot restrain the rush to judgment in the absence of reliable evidence, the proliferation of observational treatment comparisons will hinder the goal of finding effective treatments for COVID-19—and a great many other diseases.” (page 4-5)
Another factor to consider is the detrimental effects masks have on the people wearing them. Food servers, friends, and people in general have told me how much they hate wearing masks saying that they can’t breathe, have headaches, and feel exhausted after working in them all day. Still, other people have told me that wearing a mask doesn’t bother them in the least. The couple of times I wore a mask while getting a chair massage and when I went to a city hall to testify against the passage of a mask ordinance, I too felt discomfort and anxiety. In science, these statements are considered anecdotal. An anecdote is a personal narrative about how someone experiences and perceives something minus any scientific data. Sometimes anecdotal evidence is all we have to go on. When it comes to making decisions in our personal lives, it’s usually all we need. Not everything can nor probably ever will be answered via the scientific method. But when it comes to government policies like forcing people to wear masks, socially distance, etc. scientific evidence is a must.
We must breathe air to live. Without air most people would die within 3-5 minutes. Our nose and mouth were not meant to be obstructed. Obviously, masks obstruct breathing. You don’t need science to tell you that. We breathe in oxygen and exhale carbon dioxide or CO2. Carbon dioxide is a waste product of various metabolic and biochemical processes. Symptoms of not enough oxygen in the blood and tissues (hypoxemia/hypoxia) and too much CO2 in the blood (hypercapnia) include: headache, difficulty breathing, coughing, wheezing, dizziness, confusion, inability to concentrate, fatigue, panic, depression, rapid heartbeat, convulsions, hyperventilation, and death.
The WHO (World Health Organization) explicitly says not to exercise with a mask on. The CDC shamelessly tiptoes around the issue by saying that people may not be able to wear a mask while exercising if it causes difficulty breathing. But the CDC does explicitly say that anyone who has trouble breathing shouldn’t wear a mask. Also keep in mind that with a mask on you’re breathing back in bacteria and viruses that you have exhaled, some of your own CO2, any dyes and chemicals in the material the mask is made from, and if you smoke or vape your own tar and nicotine along with other toxins. Here is what the scientific literature has to say:
National Taiwan University Hospital, 2005 study from the U.S National Library of Medicine: “The Physiological impact of N95 Masks on Medical Staff.” Detailed Description: “Wearing N95 masks results in hypooxygenemia and hypercapnia which reduce working efficiency and the ability to make correct decision.” The study goes on to say: “Medical staff are at an increased risk of getting ‘severe acute respiratory syndrome’ (SARS), and wearing N95 masks is highly recommended worldwide. However, dizziness, headache, and short of breath are commonly experienced by the medical staff wearing N95 masks.” (SARS only killed 774 people worldwide)
A 2008 study on how surgical masks effect surgeons performing operations was published in Neurocirugia, the Journal of the Spanish Society of Neurosurgery (SENEC) entitled: “Preliminary report on surgical mask induced deoxygenation during major surgery.” The study was conducted on 53 surgeons 24-54 years old, non-smokers without any chronic lung disease. A pulse oximeter was used to evaluate whether their oxygen saturation of hemoglobin was affected by a surgical mask during major operations.
Introduction: “…Surgeons in the operating room frequently experience physical discomfort, fatigue, and possibly even deterioration of surgical judgment and performance…the surgeon beneath the surgical mask is often very inadequately conditioned despite the universal air conditioning standard of operating theaters. Thus they either wear masks improperly or refrain from using them altogether. As it is known that heat and moisture trapping occur beneath surgical masks, it seems reasonable that some of the exhaled CO2 may also be trapped beneath them, inducing a decrease in blood oxygenation.”
Results: “Oxygen saturation of hemoglobin decreased significantly after the operations in both age groups.” Meaning, surgeons under 35 and over 35.
Don’t confuse the Neurocirugia study with YouTube videos of surgeons and lay people sticking an oxygen meter tube under a mask they’re wearing and coming up with a reading. This is worthless for two reasons: it’s not a controlled environment and oxygen levels in the blood have to be measured at different intervals while wearing the mask. Usually, the lay people show lower oxygen levels while the doctors who are pro mask show no decrease in oxygen levels. But it doesn’t matter because devices like the ALTAIR 5X Multi Gas Detector that’s used in one of these videos weren’t designed to measure what’s going on inside a face mask.
Another problem with masks is that they are virtual breeding grounds for pathogenic microbes. A 2018 study in the Journal of Orthopaedic Translation: “Surgical masks as source of bacterial contamination during operative procedures” found:
Abstract: “This study aimed to investigate whether SMs” (surgical masks) “may be a potential source of bacterial shedding leading to an increased risk of surgical site infection.”
Methods: “We investigated the difference in bacterial counts between the SMs worn by surgeons and those placed unused in the operating room (OR), and the bacterial count variation with indicated wearing time.”
Results: “The bacterial count on the surface of the SMs increased with extended operating times…Moreover, the bacterial counts were significantly higher among the surgeons than the OR. Additionally, the bacterial count of the external surface of the second mask was significantly higher than that of the first one.”
Conclusions: “The source of bacterial contamination in SMs was the body surface of the surgeons rather than the OR environment. Moreover, we recommend that surgeons should change the mask after each operation, especially those beyond 2 hours.”
A 2019 study in BMC Infectious Diseases yielded similar results measuring viral contaminants.
A major factor in pathogenic microbes building up in masks is sweat. And what happens when people walk around wearing masks on hot humid days? They sweat. To make matters worse, just about everyone doesn’t properly wear or clean them. Instead of taking off their masks, people will be lazy and just wear them around their neck. The CDC explains this will contaminate them. Or they’ll stuff them in their pockets or purses, or they will drop them on the floor and put them back on their face. A lot of people will wear the mask below their nose, and who can blame them–they want to breathe. Go to the CDC website “How to Wear Masks” and see if you or anyone else is obsessive-compulsive enough to follow the guidelines listed there. And since most people won’t even bother to read the guidelines much less follow them, forcing people to wear masks will wind up spreading disease and poor health rather than preventing it. To quote the WHO: “Sweat can make the mask become wet more quickly which makes it difficult to breathe and promotes the growth of microorganisms.”
Bureaucrats like Anthony Fauci, Deborah Birx, CDC Director Robert Redfield, Surgeon General Jerome Adams, and the WHO know the aforementioned facts. This is why they originally advocated against wearing masks. Don’t be conned by Fauci’s baloney that he lied due to a shortage of N95 masks. He could have advised the public to wear cloth masks from the beginning. Why didn’t he? Why the 180?
In a May 27 CNN interview, Fauci said he wants masks to be “a symbol” of what we should be doing even though “it’s not 100% effective” because it shows “respect for another person.”
An April 1, 2020 article in the New England Journal of Medicine by three MDs and an RN was even more explicit: “We know that wearing a mask outside health care facilities offers little, if any protection from infection…It is also clear that masks serve symbolic roles…masks are not only tools, they are also talismans that may help increase health care workers perceived sense of safety…”
In other words, masks are worthless. Lots of viral pathogens will always get around and go through any mask. The science proving this hasn’t changed. It is the political agenda that has changed.
*
Note to readers: please click the share buttons above or below. Forward this article to your email lists. Crosspost on your blog site, internet forums. etc.
Michael J. Talmo has been a professional writer for over 40 years and is strongly committed to the protection of civil liberties. He can be reached at [email protected].


