Non-Alcoholic Fatty Liver Disease (NAFLD) Has Become a Health Emergency Among Children

All Global Research articles can be read in 51 languages by activating the Translate Website button below the author’s name.
To receive Global Research’s Daily Newsletter (selected articles), click here.
Click the share button above to email/forward this article to your friends and colleagues. Follow us on Instagram and Twitter and subscribe to our Telegram Channel. Feel free to repost and share widely Global Research articles.
***
NAFLD is characterized by excess fat buildup in your liver. Without proper treatment, it can lead to serious liver problems including nonalcoholic steatohepatitis (NASH), which causes inflammation and fibrosis, or scarring of the liver. NAFLD also increases the risk of other health conditions, including cardiovascular disease
The first documented cases of nonalcoholic fatty liver disease (NAFLD) didn’t come about until 1980. Today, NAFLD affects 32.4% of people globally, and it’s the most common cause of liver transplant in adults under the age of 50
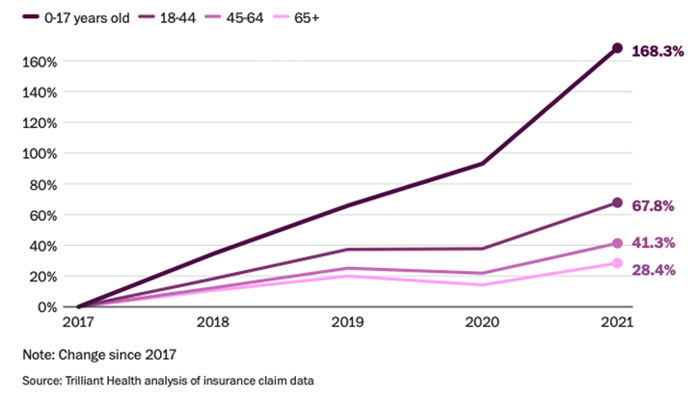
NAFLD also affects up to 9.6% of American children aged 2 to 19, making it as common as asthma. In 15- to 19-year-olds, prevalence is as high as 17.3%. Prevalence among children 0 to 17 has risen 168.3% since 2017, with a particularly precipitous rise starting in 2020
The dramatic rise in NAFLD in early 2020 may in part be due to the COVID lockdowns, which had the effect of raising childhood obesity rates by 8.3% to 13.4%, depending on the age group
Maternal obesity and high consumption of diet soda and/or junk food during pregnancy have both been linked to NAFLD in offspring, and one theory is that artificial sweeteners may be programming the metabolism of the fetus to favor fat storage over energy production
*
Fatty liver disease used to be a disease seen almost exclusively in the elderly, primarily heavy drinkers. The first documented cases of nonalcoholic fatty liver disease (NAFLD) didn’t come until I was in medical school in 1980.1 At the time, the researchers described it as a “hitherto unnamed liver disease of unknown cause.”
In June 2023, scientists proposed rebranding NAFLD to “metabolic dysfunction-associated steatotic liver disease,” to highlight its relation to other metabolic conditions such as diabetes. What connects all metabolic conditions is that your body is not converting food to energy in an efficient manner.
In the video above, independent health researcher Jay Feldman investigates the true causes of NAFLD. This is Part 2 of an eight-part series. It’s like a master’s course on NAFLD, as he goes over virtually everything you could possibly want or need to know about it. If you or someone you know is currently struggling with NAFLD, I strongly encourage you to view all eight episodes.
In the featured episode, he explains why fructose is NOT the main culprit as commonly thought, how your liver produces fat from both fructose and dietary fats, and how impaired energy production in your mitochondria results in NAFLD.
What Is NAFLD?
NAFLD is characterized by excess fat buildup in your liver. Without proper treatment, it can lead to serious liver problems including nonalcoholic steatohepatitis (NASH), which causes inflammation and fibrosis, or scarring of the liver.
NASH may lead to cirrhosis, which increases the risk of liver cancer, and end-stage liver disease. NAFLD also increases the risk of other health conditions, including cardiovascular disease, which is the No. 1 cause of death in people with NAFLD. NAFLD often has no symptoms, although it may cause fatigue, jaundice, swelling in the legs and abdomen, mental confusion and more.
Your liver carries out more than 500 functions that are essential for health. This includes the production of bile (which breaks down dietary fats and carries away waste), converting excess glucose into glycogen, and regulating amino acids in the blood. It’s also important for detoxification, helping to clear your blood of toxins.
The good news is that your liver, more than almost any other tissue in your body, has phenomenal regeneration capabilities. Even if 90% of it has been removed, it can regrow to its normal size. NAFLD can also be successfully reversed in its early stages via lifestyle changes, like healthy eating and exercising.
NAFLD Prevalence Has Skyrocketed
Today, NAFLD affects 32.4% of people globally,2 and it’s the most common cause of liver transplant in adults under the age of 50.3 NAFLD also affects up to 9.6% of American children aged 2 to 19,4making it as common as asthma.5 In 15- to 19-year-olds, prevalence is as high as 17.3%.6
What’s particularly strange is that the skyrocketing prevalence in children and teens is quite new. As illustrated in the graph below from Trilliant Health,7 prevalence of NAFLD has risen 168.3% since 2017, with a particularly precipitous rise starting in 2020.
Obesity Is a Primary Risk Factor for NAFLD
As reported in a March 2021 paper on pediatric NAFLD:8
“The largest risk factor for NAFLD is obesity. Obesity and NAFLD in children are often associated; however, they are not concomitant.
In a 2019 study in 408 children with obesity using whole liver magnetic resonance imaging–proton density fat fraction, the prevalence rate of NAFLD was 26.0%, or roughly one in every four children. In the Teen LABS study of adolescents with obesity severe enough to warrant weight loss surgery, the prevalence rate of NAFLD was higher at 59%.”
The dramatic rise in NAFLD in early 2020 may in part be due to the COVID lockdowns, which had the effect of raising childhood obesity rates by 8.3% to 13.4%, depending on the age group.9
Artificial Sweeteners May Impair Metabolism
That said, NAFLD also occurs in an estimated 8% of normal weight children.10 Inherited predisposition may be part of the problem. But the environment in utero can also influence a child’s risk of NAFLD,11 and this is a far more likely explanation for the recent explosion in prevalence among children.
Maternal obesity and high consumption of diet soda and/or junk food during pregnancy have both been linked to NAFLD in offspring, and one theory is that artificial sweeteners may be programming the metabolism of the fetus to favor fat storage over energy production.12
Babies are also routinely fed unnaturally high amounts of sweeteners in infant formula and baby food. In recent years, the baby formula industry has started marketing formula made with corn syrup solids instead of lactose from cow’s milk. It’s said to be better for babies with sensitivity to lactose.
However, recent research13 suggests formula made with corn syrup solids significantly increases your child’s risk of obesity by age 4, and by extension NAFLD, and those who consume the highest amounts of formula have the highest risk.
So-called “transition formula” and “toddler milk” also contain higher amounts of sugar than regular cow’s milk. Both products are pure marketing inventions that have no nutritional basis. Meanwhile, research14 has shown that consumption of unsweetened cow’s milk is associated with a lower risk of NAFLD.
The Role of Diet
Indeed, our modern diet is probably the most important driver of this condition. As reported by The Washington Post:15
“… many doctors believe that our modern lifestyle — diet, the increase in sedentary activities related to technology and environmental exposures — is to blame. One of the liver’s jobs is to filter toxins, and when something in the body is out of balance, the organ can become damaged and fail …
A little fat in the liver is normal, but when more than 5% of its cells contain fat, the organ’s ability to do its job is impeded, and pediatric specialists say some children they treat have livers with 30 to 40% or even as high as 60% fat …
Some pediatric experts theorize there’s a mismatch between our genetics and the highly processed and sugary foods that have come to dominate childhood diets.
Nutritional surveys show that meals eaten by kids changed radically in a generation, going from very little ultra-processed foods in the early 1980s … to more than 67%16 in recent years. Such diets lead to hormonal changes and other stresses on our bodies.
‘It creates a time bomb, and it is killing our kids,’ said Barry M. Popkin, a professor of nutrition at the Gillings School of Global Public Health at the University of North Carolina at Chapel Hill.”
The Washington Post goes on to cite a January 2022 systematic review17 that found “a parallel but delayed rise” in noncommunicable diseases with rising prevalence of ultraprocessed foods.
Between 1800 and 2019, processed and ultraprocessed foods rose from less than 5% to more than 60%. This radically altered the macronutrient content of our diets. Sugar and seed oil (or “vegetable oil”) consumption rose dramatically, while saturated fat from animals dropped.
Ditch the Fast Food to Protect Your Child’s Health
Of these, I believe the transition from saturated animal fats to seed oils has played the biggest role. As detailed in “Linoleic Acid — The Most Destructive Ingredient in Your Diet,” seed oil is the primary source of linoleic acid (LA), which destroys your mitochondrial function.
I’m convinced excessive LA consumption is the biggest contributor to chronic disease in the Western world, including NAFLD. To understand how LA undermines your health, and that of your children, please read through that article and watch the video included in it. Both provide a comprehensive overview of how LA drives chronic disease of all kinds.
To avoid LA, you’ll need to avoid processed foods, fast foods and most restaurant foods, and focus on real, whole, organically grown foods instead. Processed foods are also routinely contaminated with glyphosate, which can contribute to liver problems. Disturbingly, recent testing revealed 95% of school lunch items had detectable levels of glyphosate,18 so, if at all possible, provide your child with homemade lunches.
A shocking 100% of meals also contained heavy metals at levels up to 6,293 times higher than the maximum levels allowed in drinking water. Meanwhile, most of the meals were “abysmally low” in essential nutrients.
Fast food also contains extremely low amounts of essential nutrients, especially B vitamins. In fact, zero amounts of vitamin B9 or B12 were detected in the top 10 fast foods sampled.19
That’s rather remarkable, considering B12-rich foods include beef and chicken, both of which are staples in fast food, yet fast food beef and chicken provide no B12 at all! If that doesn’t convince you that fast food meat is nowhere near the same as grass fed organic meat, I don’t know what will.
Fatty liver can also be driven by excess sugar when, in addition to seed oils, you are consuming more than 35% or so of your calories as fat. This is likely why this condition is now found even in young children.
Nutrients That Help Combat NAFLD
Upping your intake of specific nutrients can also be helpful if you have NAFLD. Examples include:
Choline — Choline is important for normal liver function and liver health by moving fat out of your liver. It also helps maintain membrane integrity and manages cholesterol metabolism, including low density lipoproteins (LDL) and very low-density lipoproteins (VLDL). Choline deficiency has been shown to enhance abnormal fat deposits in your liver, causing NAFLD.20
In fact, some experts believe NAFLD is largely the result of shunning choline-rich foods like liver and egg yolks,21 which is then worsened by consuming too much LA. You can increase your intake by consuming more choline-rich foods, such as organic pastured egg yolks, grass fed beef liver, wild-caught Alaskan salmon and krill oil. Arugula is also an excellent source.
Vitamin B12 and folic acid may also be protective and have been found to decrease the progression of NASH.22
Niacinamide, also known as nicotinamide (NAM) — Niacinamide is a precursor to nicotinamide adenine dinucleotide (NAD+), a vital signaling molecule that’s believed to play an important role in longevity. Supplementation has also been found to decrease oxidative stress and prevent fatty liver.23
N-acetylcysteine (NAC) — NAC is a precursor needed for glutathione biosynthesis. It’s used as an antidote for acetaminophen toxicity, which causes liver damage by depleting glutathione. Research published in Hepatitis Monthly has shown NAC supplementation helps improve liver function in patients with NAFLD.24
Milk thistle — This herb contains silymarin and silybin, antioxidants that are known to help protect your liver from toxins and even help regenerate liver cells.25
CoQ10 — CoQ10 keeps your mitochondria healthy and plays a crucial role in the production of ATP, the cellular energy required to keep you alive. Supplementing with CoQ10, or the natural form called ubiquinol, has been shown to improve NAFLD by reducing oxidative stress and inflammation.26
Remember that supplements should always be used in combination with a healthy lifestyle, including eating right and exercising. If you’re overweight, losing 7% to 10% of your body weight can improve NAFLD, including lowering liver fat content, liver inflammation and fibrosis.27
*
Note to readers: Please click the share button above. Follow us on Instagram and Twitter and subscribe to our Telegram Channel. Feel free to repost and share widely Global Research articles.
Notes
1, 5, 7, 12, 15 Washington Post October 3, 2023 (Archived)
2 The Lancet Gastroenterology & Hepatology September 2022; 7(9): 851-861
3, 4, 6, 8, 10, 11 Clinical Liver Disease March 2021; 17(3): 196–199
13 American Journal of Clinical Nutrition October 2022; 116(4): 1002–1009
14 Frontiers in Nutrition 2023; 10: 1119118
17 Frontiers of Nutrition January 13, 2022
18 Moms Across America September 28, 2022
19 Moms Across America October 18, 2023
20 Oregon State University Linus Pauling Institute
21 chrismasterjohnphd.com November 23, 2010
22 Journal of Hepatology, 2022; doi: 10.1016/j.hep.2022.06.033
23 The Journal of Nutritional Biochemistry May 21, 2022
24 Hepatitis Monthly, 2010; 10(1):12
25 Indian J Biochem Biophys. 2006 Oct;43(5):306-11
26 Journal of Prescribing Practice. 2020;2(4)
27 Curr Obes Rep. 2019 Sep; 8(3): 220–228
Featured image is from Fitterfly

