Letter to Physicians: Four New Scientific Discoveries Regarding the Safety and Efficacy of COVID-19 Vaccines
All Global Research articles can be read in 51 languages by activating the “Translate Website” drop down menu on the top banner of our home page (Desktop version).
Visit and follow us on Instagram at @crg_globalresearch.
***
Doctors for Covid Ethics has sent the following letter to tens of thousands of doctors in Europe, summarising four recent scientific findings critical to the COVID-19 vaccination program. The letter explains each finding as it relates to the biology of COVID-19 vaccines, including interactions with the immune system.
Taken together, the letter warns that these new pieces of evidence force all physicians administering COVID-19 vaccines to re-evaluate the merits of COVID-19 vaccination, in the interests of their own ethical standing, and their patients’ safety and health.
A video explanation of the underlying immunology by Professor Sucharit Bhakdi MD is here, with German subtitles here.
*
Dear Colleague:
Four recent scientific discoveries are herewith brought to your urgent attention. They alter the entire landscape of the COVID-19 pandemic, and they force us to reassess the merits of vaccination against SARS-CoV-2.
Summary
Rapid and efficient memory-type immune responses occur reliably in virtually all unvaccinated individuals who are exposed to SARS-CoV-2. The effectiveness of further boosting the immune response through vaccination is therefore highly doubtful. Vaccination may instead aggravate disease through antibody-dependent enhancement (ADE).
Discovery 1: SARS-CoV-2 spike protein circulates shortly after vaccination
SARS-CoV-2 proteins were measured in longitudinal plasma samples collected from 13 participants who received two doses of Moderna mRNA-1273 vaccine [1]. With 11 of the 13, the SARS-CoV-2 spike protein was detected in the blood within only one day after the first vaccine injection.
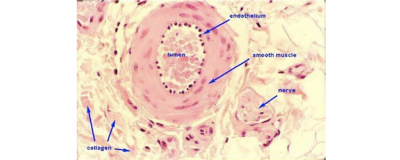
Significance. Spike protein molecules were produced within cells that are in contact with the bloodstream—mostly endothelial cells—and released into the circulation. This means that a) the immune system will attack those endothelial cells, and b) the circulating spike protein molecules will activate thrombocytes. Both effects will promote blood clotting. This explains the many clotting-related adverse events—stroke, heart attack, venous thrombosis—that are being reported after vaccination.
Discovery 2: Rapid, memory-type antibody response after vaccination
Several studies have demonstrated that circulating SARS-CoV-2-specific IgG and IgA antibodies became detectable within 1-2 weeks after application of mRNA vaccines [1–3].
Significance. Rapid production of IgG and IgA always indicates a secondary, memory-type response that is elicited through re-stimulation of pre-existing immune cells. Primary immune responses to novel antigens take longer to evolve and initially produce IgM antibodies, which is then followed by the isotype switch to IgG and IgA.
A certain amount of IgM was indeed detected alongside IgG and IgA in some studies [1,4]. Importantly, however, IgG rose faster than IgM [4], which confirms that the early IgG response was indeed of the memory type. This memory response indicates pre-existing, cross-reactive immunity due to previous infection with ordinary respiratory human coronavirus strains. The delayed IgM response most likely represents a primary response to novel epitopes which are specific to SARS-CoV-2.
Memory-type responses have also been documented with respect to T-cell-mediated immunity [5–7]. Overall, these findings indicate that our immune system efficiently recognizes SARS-CoV-2 as “known” even on first contact. Severe cases of the disease thus cannot be ascribed to lacking immunity. Instead, severe cases might very well be caused or aggravated by pre-existing immunity through antibody-dependent enhancement (ADE, see below).
Discovery 3: SARS-CoV-2 elicits robust adaptive immune responses regardless of disease severity
Serum antibody profiles were reported for 203 individuals following SARS-CoV-2 infection [8]. 202 (>99%) of the participants exhibited SARS-CoV-2 specific antibodies. With 193 individuals (95%), these antibodies prevented SARS-CoV-2 infection in cell culture and also inhibited binding of the spike protein to the ACE2 receptor. Furthermore, CD8+ T-cell responses specific for SARS-CoV-2 were clear and quantifiable in 95 of 106 (90%) HLA-A2-positive individuals.
Significance. This study confirms the above assertion that the immune response to initial contact with SARS-CoV-2 is of the memory type. In addition, it shows that this reaction occurs with almost all individuals, and particularly also with those who experience no manifest clinical symptoms.
The goal of the vaccination is to stimulate production of antibodies to SARS-CoV-2, but we now know that such antibodies can and will be rapidly generated by everyone upon the slightest viral challenge, even without vaccination.
Severe lung infections always take many days to develop, which means that if the antibodies generated by the memory response are needed, they will arrive on time. Therefore, vaccination is unlikely to provide significant benefit with respect to the prevention of severe lung infection.
Discovery 4: Rapid increase of spike protein antibodies after the second injection of mRNA vaccines
IgG and IgA antibody titres were monitored before vaccination and after the first and the second injection of mRNA vaccines [3]. Antibody titres rose with some delay after the first injection, then plateaued, but rose again very shortly after the second injection.
Significance. Even though the antibody response to the first injection is of the memory type, the small time lag after the injection may mitigate adverse reactions, because the abundance of spike protein on the cells in the blood vessel walls and in other tissues may have already passed its peak when the antibodies arrive.
The situation changes dramatically with the second injection. Then the spikes are produced and protrude into the bloodstream that is already swarming with both reactive lymphocytes and antibodies. The antibodies will cause the complement system [9,10] and also neutrophil granulocytes to attack the spike protein-bearing cells. The possible consequences of all-out self-attack by the immune system are frightening.
Antibody-dependent enhancement of disease
As described, memory-type immune responses ensure the rapid rise of antibody titres after initial exposure to SARS-CoV-2, rendering the benefit of vaccine-induced antibody response exceedingly doubtful. Regardless, we should not assume that high antibody titres against SARS-CoV-2 will always improve the clinical outcome. With several virus families—in particular with Dengue virus, but also with coronaviruses—antibodies can aggravate rather than mitigate disease. This occurs because certain cells of the immune system take up antibody-tagged microbes and destroy them. If a virus particle to which antibodies have bound is taken up by such a cell, but it then manages to evade destruction, it may instead start to multiply within the cell. Overall, the antibody will then have enhanced the replication of the virus. Clinically, this antibody-dependent enhancement (ADE) can cause a hyperinflammatory response (a “cytokine storm”) that will amplify the damage to the lungs, liver and other organs of our body.
Attempts to develop vaccines to the original SARS virus, which is closely related to SARS-CoV-2, repeatedly failed due to ADE. The vaccines did induce antibodies, but when the vaccinated animals were subsequently infected with the virus, they became more ill than the unvaccinated controls (see e.g. [11]). The possibility of ADE was not adequately addressed in the clinical trials on any of the COVID-19 vaccines. It is therefore prudent to avoid the danger of inducing ADE through vaccination and instead rely on proven forms of treatment [12] for dealing with clinically severe COVID-19 disease.
Conclusion
The collective findings discussed above clearly show that the benefits of vaccination are highly doubtful. In contrast, the harm the vaccines do is very well substantiated, with more than 15.000 vaccination-associated deaths now documented in the EU drug adverse events database (EudraVigilance), and over 7.000 more deaths within the UK and the US [13].
ALL PHYSICIANS MUST RECONSIDER THE ETHICAL ISSUES SURROUNDING COVID-19 VACCINATION.
*
Note to readers: Please click the share buttons above or below. Follow us on Instagram, @crg_globalresearch. Forward this article to your email lists. Crosspost on your blog site, internet forums. etc.
Notes
1. Ogata, A.F. et al. (2021) Circulating SARS-CoV-2 Vaccine Antigen Detected in the Plasma of mRNA-1273 Vaccine Recipients. Clin. Infect. Dis. -:x-x
2. Amanat, F. et al. (2021) SARS-CoV-2 mRNA vaccination induces functionally diverse antibodies to NTD, RBD and S2. Cell -:x-x
3. Wisnewski, A.V. et al. (2021) Human IgG and IgA responses to COVID-19 mRNA vaccines. PLoS One 16:e0249499
4. Qu, J. et al. (2020) Profile of Immunoglobulin G and IgM Antibodies Against Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Clin. Infect. Dis. 71:2255-2258
5. Le Bert, N. et al. (2020) SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls. Nature 584:457-462
6. Grifoni, A. et al. (2020) Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals. Cell 181:1489-1501.e15
7. Gallais, F. et al. (2021) Intrafamilial Exposure to SARS-CoV-2 Associated with Cellular Immune Response without Seroconversion. Emerg. Infect. Dis. 27:x-x
8. Nielsen, S.S. et al. (2021) SARS-CoV-2 elicits robust adaptive immune responses regardless of disease severity. EBioMedicine 68:103410
9. Magro, C.M. et al. (2020) Docked severe acute respiratory syndrome coronavirus 2 proteins within the cutaneous and subcutaneous microvasculature and their role in the pathogenesis of severe coronavirus disease 2019. Hum. Pathol. 106:106-116
10. Magro, C.M. et al. (2021) Severe COVID-19: A multifaceted viral vasculopathy syndrome. Annals of diagnostic pathology 50:151645
11. Tseng, C. et al. (2012) Immunization with SARS coronavirus vaccines leads to pulmonary immunopathology on challenge with the SARS virus. PLoS One 7:e35421
12. McCullough, P.A. et al. (2021) Pathophysiological Basis and Rationale for Early Outpatient Treatment of SARS-CoV-2 (COVID-19) Infection. Am. J. Med. 134:16-22
13. Johnson, L. (2021) Official Vaccine Injury and Fatality Data: EU, UK and US.
Featured image is from Doctors for COVID Ethics

