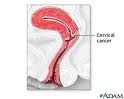
Cervical Cancer can be Prevented
Yet 13,000 women in the US get it
While one of the singular achievements of American medicine in recent years has been to reduce the largely preventable incidence of cervical cancer, 13,000 women nevertheless will come down with it this year mainly because they have not had a Pap smear to detect it. As the disease ordinarily takes about 10 years to progress, “cervix cancer happens to be a cancer that you can use screening techniques to try to pick up early” and treat, says Dr. Ursula Matulonis, of Boston’s Dana-Farber Cancer Institute. Globally, about 40 percent of the 500,000 women stricken with the disease will die for lack of a proper medical treatment, she says. That’s because women in some countries do not routinely get Pap smears and when the transmitting agent, human papillomavirus(HPV), infects the cervix it does not get treated because of society’s inadequate medical infrastructure. When the disease is undetected and allowed to grow, the victims will suffer pain and bleeding as the cancer spreads. It is caused by one of the 75 types of HPV, a ubiquitous virus that is present in both men and women and which causes 95 percent of the cancers.
Compared to other forms of cancer, the cervical form is still a relatively rare tumor, Dr. Matulonis says. Ovarian cancer afflicts 25,000 American women annually; breast cancer, 180,000 women; and lung cancer about 200,000 women. Since the cervical form can be detected early and treated successfully, the number of women who have Stage IV cervical cancer “should be zero,” she says. Even though the death rate from cervical cancer has been declining by 4 percent a year, the grim news is that, according to the National Cervical Cancer Coalition of West Hills, Calif., more than 4,000 American women die of the disease annually. Many of them are of the 11 percent of U.S. women who do not have Pap screenings.
The Pap test is used by gynaecologists to detect any premalignant or malignant cells gathered from the outer opening of the cervix and examined for abnormalities. In general, observes Wikipedia, the test is recommended for women aged 25 to 65 who have had sex. “Most women contract HPV soon after becoming sexually active. It takes an average of a year, but can take up to four years, for a woman’s immune system to control the initial infection. Screening during this period may show this immune reaction and repair as mild abnormalities, which are usually not associated with cervical cancer, but could cause the woman stress and result in further tests and possible treatment,” Wikipedia says.
“It’s important for folks to know that you do not have to have intercourse to spread the virus, but that the virus could be spread just by skin-to-skin contact,” Dr. Matulonis warns, explaining that the virus “probably gets into the cervix cells just by small breaks in the skin.” Dr. Matulonis made her comments in an interview with law Professor Diane Sullivan for the Comcast SportsNet broadcast “Educational Forum,” produced by the Massachusetts School of Law at Andover. “Worldwide, HPV is the most common sexually transmitted infection in adults,” Wikipedia reports, noting that more than 80 percent of American women will have contracted at least one strain of HPV by age fifty.
“Accordingly, public health officials in Australia, Canada, Europe, and the United States recommend vaccination of young women against HPV,” Wikipedia notes. As the vaccine only covers some strains of HPV, medical authorities still urge regular Pap smear screening even after vaccination. Doctor Matulonis says the vaccine is essentially mimicking the virus, giving the individual a fraction of the virus so that one’s immune system can mount a response “to certain proteins that are present in that virus.” She goes on to say, “It’s important to remember that for any vaccine to work properly and effectively that that vaccine is given to somebody before they’re exposed to the virus.”
Tracing the progress of the disease, Dr. Matulonis says (1) the first piece of HPV’s wrongdoing is the person becoming infected; (2) the virus persistently stays with the cervix cells; (3) the individual reaches a point of preinvasive disease, “meaning not quite cancer but the step just before it,” where preinvasive changes take place on the cervix; and (4) invasive cervical cancer. In all, the process takes about 10 years to become cancerous.
Asked if vaccinating all young girls would reduce the incidence of cervical cancer to zero, Dr. Matulonis replied there is much about the new vaccines that remain unknown. “We don’t know that the vaccines will be excellent at reducing the persistence of HPV infection…So if you have a vaccine that looks at HPV16 and HPV18 (two of the strains of HPV) you can really nicely see that those women vaccinated do not have persistent infections and they do not have persistent changes within the cervix called CIN2 or CIN3 that are indicative of that type of infection. But we haven’t gotten to the point where we can say, ‘Look, we’ve now been able to reduce the number of cervical cancer cases’ (although) I bet that’s going to happen because you’ve got a reduction in the abnormal Pap smear rate…”Another important point is that if a girl is vaccinated at 10 “Do you need a booster vaccine? We don’t know,” Matulonis says. “We don’t know how long the vaccine will produce antibodies against the different proteins within the HPV16 and HPV18. The persistence of the vaccine is not known.”
Other questions about the vaccine persist as well. “’Is it possible that the HPV virus will change its look so that it might survive despite the vaccine?’” Dr. Matulonis asks. “Unknown question. ‘Should we be vaccinating boys?’ Also not known. Another important question is ‘If you’re not nine or 20 but if you’re 25 or 26 and you have been sexually active, how effective is the vaccine?’ We do know that when somebody has become sexually active that the vaccine does not work as well. This doesn’t mean that it doesn’t work but the reduction in the abnormal Pap smear rates is not as robust compared to when you vaccinate somebody before they become sexually active.”
Asked about possible obstacles to widespread implementation of a vaccine program, Dr. Matulonis pointed out that the Food and Drug Administration(FDA) has recommended that young girls be vaccinated as early as age nine most of them will be seen by their pediatricians. “So pediatricians will be a potential barrier to vaccination, depending upon whether or not they believe the studies, ethical concerns, social concerns, so they’ll be a barrier. Potentially, the nursing staff with the medical offices may be a barrier. Again, these may not be barriers—but we just don’t know yet.” She adds that as girls mature they will have more to say about their own medical care, “so they’re going to be very potentially involved in the decision whether or not they get vaccinated. (They’re) going to be exposed to the advertising campaigns that are out there for these vaccines and will be educated about HPV and what causes cervical cancer. And obviously, lastly but not leastly, will be the parents.”
Women who smoke and take oral contraceptives, she says, are adding co-factors that will increase their chances of getting invasive cervical cancer. “There’s something about smoking and the ability to clear the virus, so that (promotes the) second step on the way to cervical cancer, so after the virus penetrates the cervix, it sets up shop and if somebody smokes a lot the immune system may not be able to clear the virus,” Dr. Matulonis says. Plus, a new report suggests women who take oral contraceptives are at a slightly higher risk of cervical cancer, she adds. This “probably has something to do with the hormones in the oral contraceptives that might make HPV last a little bit longer in the cervix. Once you stop the oral contraceptives, just as when you stop oral contraceptives for menopausal symptoms, that risk of cancer drops away.”
Faith Morgida, an attorney and graduate of the law school who developed cervical cancer, said it was detected by her annual Pap smear. Morgida, aged 52, told interviewer Sullivan that she was considering reducing the frequency to every other year because “it’s not a fun type examination” but that she is happy she kept to the annual regimen. When her smear came back abnormal, Morgida asked for the exam to be repeated and it, too, proved abnormal, with a report of a high number of squamous cells. Morgida was also tested for the presence of HPV, also found to be present. The attorney next had a colposcopy procedure, where doctors looked at her cervix and reproductive system through a microscope to detect any abnormal cells. They performed manual biopsies, sending the tissue snippets to a pathology lab for further testing. The resultant report showed the presence of cervical cancer and also precancerous cells, plus HPV in her system.
Following this diagnosis, Morgida’s oncologist performed a Loop Electrosurgical Excision Procedure, or LEEP. This involves cauterizing the malignant cells with an electrified wire fashioned in a loop atop a long, pencil-like device. The patient is grounded as the machine is part electrical generator as well as part microscope. Morgida recalls thinking “it’s kind of something out of Frankenstein but it’s so less invasive than actually cutting into you” and it is done with a local aesthetic. Morgida was told afterwards biopsies showed her that if her cells were not already cancerous they were at the least precancerous but that the procedure had removed them. For now, Morgida gets a pap smear every three months so that her physician can determine if any abnormal cells are coming back. “I grew up in an era when anybody who had cancer it was like a death sentence,” she recalled. “And it’s hard to get over that fear even though you know many many people who have had cancer and beaten it. The minute you hear the C word you think, ‘Oh, God, my life is over’ and then you have to step back and say, ‘OK, listen to your doctors.’” She adds, “A LEEP procedure isn’t that bad. I was worried about the pain level. I was worried about the unknown. Don’t worry, take it one step at a time.”
Law professor Constance Rudnick of Massachusetts School of Law at Andover, told host Sullivan that 24 states and the District of Columbia have introduced some kind of legislation relating to HPV. “There were very few (states) that are mandatory,” that is making school attendance conditional on receiving the vaccine. “Some deal with education, requiring information to be disseminated. Some are just funding legislation, which on a voluntary basis would pay for the vaccine, which is relatively costly,” she said. But when the Governor Rick Perry of Texas issued an order saying all young girls would have to be vaccinated a fairly large public outcry caused the Legislature to override his executive order. The governor’s plan had been to require all girls going into the sixth grade to be vaccinated with three doses of Gardasil, a Merck and Co. product, over a six-month period. The $360 cost would be covered by most insurance plans and the State would pay for those without coverage. The announcement caused upset parents to light up the telephone lines of State Senator Jane Nelson, chairman of the Committee on Health and Human Services, who said the idea was adopted without discussion or debate.
Rudnick says challenges to the legality of vaccination stem from proponents of parental rights. Their view is that the Constitution protects the right of parents to raise their children in a manner which they see fit, particularly when it comes to sexuality.” What’s more, “The right of free exercise of religion plays into this kind of instruction, and there are some religions whose principles are based on abstinence prior to marriage—and the belief was that if you vaccinate young girls they would become more sexually active prior to marriage, and therefore there’s a potential freedom of religion violation as well,” she adds.
Rudnick notes, “almost all states have a religious exemption to vaccination—measles, smallpox, the kind of vaccinations we’re more familiar with to prevent childhood illnesses, polio, tetanus, and the like. So proponents say, ‘Hey, we’ve been doing this for years with respect to other communicable diseases (so) this shouldn’t be such a big deal.’” But opponents say HPV vaccine differs, from polio prevention in that “HPV is not contagious except through sexual contact and those other diseases do not involve sex by young girls who may be, in many cases, below the age of consent, which would make the sexual activity a crime. So they’re very, very different,” Rudnick says.
Additionally, Rudnick points out, is a growing concern about the efficacy and reliability of the vaccine. Recently, one young woman claimed she was paralyzed by it. “So I think, quite frankly, in the long run the major issue is going to be effectiveness and personal risk.” Morgida, though, believes they should start inoculations at the age of 14 or 15, particularly as insurance encourages it and the American Health Association encourages it up until the age of about 35 or 40. “Even women who have had sex once in their life or practice safe sex can catch it. It’s not something that wearing a condom will necessarily prevent. So women can be at risk, very very sexually safe women can be at risk…And if you can get a vaccine that will help you beat a huge factor of cervical cancer and other reproductive cancers, why not do that?”
Federal vaccine advisers lately have been deciding whether vaccines against sexually transmitted infections “should be used more widely in boys and young men,” The New York Times reported on October 29th, 2010. “Concerns about whether to vaccinate against a sexually transmitted disease are made even more charged because much of the serious disease results from homosexual sex. The advisers must also decide whether vaccinating boys would divert scarce resources from a vaccination campaign for girls that has had poor results.”
The Massachusetts School of Law at Andover was founded in 1988 to provide an affordable, quality education to students from minority, immigrant, and low-income backgrounds who would not otherwise be able to afford the cost of a legal education. It also serves to provide through its publications and television broadcasts information on critical public issues. To interview either professor Sullivan or Rudnick, call them at (978) 681-0800. Reach Sherwood Ross, media consultant to the law school, at [email protected]

