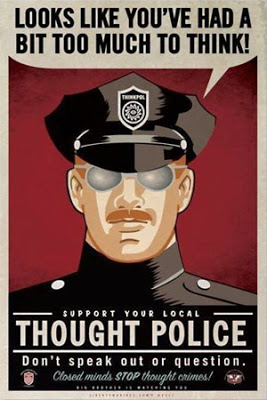
Predictive Technology: A New Tool For The Thought Police
Predictive technology is exploding, in stealth, across the virtual landscape. The arrival of Big Data initiatives by government, as well as a massive industry of data brokers is not only putting privacy at risk, but is offering those with access to the information unprecedented ways to manage the lives of everyday citizens.
Until this point, it has been a very tech-heavy subject inclined to produce glazed eyes when addressed. However, the viral story of Facebook using their algorithms to go beyond surveillance and actually manipulate the emotions of users as a type of psychology experiment has thrust these practices into the mainstream.
Certainly this experiment being conducted without the knowledge or consent of those involved is a huge breach of privacy and ethics. However, when it comes to policing and health, things really are turning Orwellian as thought “crimes” are now detectable with predictive technology.
The emergence of predictive policing and predictive healthcare has a single benefit that the Facebook example does not: the PR push that their tools are making people safer. Thus, the notion of Minority Report-style pre-crime has become a reality in both Illinois and California with no where near the pushback that is being expressed toward Facebook.
Concurrently, the medical field is merging with an array of wearable gadgetry that is flooding the consumer marketplace with millions of sensors to track vital signs in real time. Through the promise of both personal health attainment and medical threat alerts, people are embracing this tech in droves.
However, if you thought you were only monitoring yourself to perhaps make better personal choices, think again. A Bloomberg headline states: “Your Doctor Knows You’re Killing Yourself. The Data Brokers Told Her.” The article details what the data already shows about how your consumer purchases might indicate your lifestyle health index.
You may soon get a call from your doctor if you’ve let your gym membership lapse, made a habit of picking up candy bars at the check-out counter or begin shopping at plus-sized stores.
That’s because some hospitals are starting to use detailed consumer data to create profiles on current and potential patients to identify those most likely to get sick, so the hospitals can intervene before they do. Information compiled by data brokers from public records and credit card transactions can reveal where a person shops, the food they buy, and whether they smoke. The largest hospital chain in the Carolinas is plugging data for 2 million people into algorithms designed to identify high-risk patients, while Pennsylvania’s biggest system uses household and demographic data. (emphasis added)
Now imagine giving them real-time data about your vital signs on top of that.
As Jon Rappoport detailed, this type of information is irresistible to control systems that are ripe for corruption. Embedded in the Patient Protection and Affordable Care Act (aka Obamacare), there lies disturbing verbiage indicating that the personal options arising from wearable gadgets and consumer behavior may become government mandated in the near future. He cites two key quotes from a Managed Care article,“More Data in Health Care Will Enable Predictive Modeling Advances.”
Predictive modeling (PM) has grown to be a linchpin of care management. Health plans, integrated delivery systems, and other health care organizations (HCOs) increasingly channel their patients to interventions based in part on what they deduce from predictive models that have traditionally been run against databases of administrative claims. In this arena, the Affordable Care Act (ACA) [Obamacare] is likely to exert a profound effect.
…a growing number of health care experts, including the Care Continuum Alliance, see predictive modeling as an opportunity to prevent [disease] complications, control [hospital] readmissions, generate more precise diagnoses and treatments, predict risk, and control costs for a more diverse array of population segments than previously attempted. (emphasis added)
Mental health, of course, would not be excluded. This is where the entire surveillance-security-health complex begins to merge. Rappoport envisions the following scenario:
Oh, yes, in USA population sector A-2ab, we can view the electronic health records of 10,000 patients who are single, under 30, live at home with their parents, have a history of ignoring medical advice, display symptoms of ADHD, graduated college with less than a 3.0 grade average, have taken prescription pain meds within the last five years…according to statistics, this group stands a better than 65% chance of developing clinical depression within the next 6.23 years. Therefore, we should prescribe them prophylactic antidepressants now, to save money on more expensive treatments later. If we utilize our algorithm and adjust code 4aQ1 and code 7B2Ex, we’ll be able to pinpoint which patients in this group need medication immediately…
A recent report by NBC made the above fiction plausible. In a stunning admission, NBC reveals that Arizona police have a “Mental Health Support Team” that is prepared to involuntarily lock up people who seem likely to snap and commit acts of violence. These mental health police units look to harvest everything from medical records to gun purchases to online posts.
Now armed with data brokers, artificial intelligence algorithms, health databases merged with police, and the political will to implement all of it, we arrive at the latest: “Smartphone App May Revolutionize Mental Health Treatment.” The app has been developed by Tel Aviv University in Israel. The full press release must be read to be believed, as it reveals the crux of where all of this is heading (emphasis and parentheses mine).
Mental illness accounts for 90 percent of all reported suicides and places the largest burden of any disease on social and economic infrastructures worldwide, according to the World Health Organization. There is a dire need for support services to assist clinicians in the evaluation and treatment of those suffering from mental illness.
New technology developed by researchers at Tel Aviv University is poised to transform the way in which patients with mental illnesses are monitored and treated by clinicians.
Dr. Uri Nevo, research team engineer Keren Sela, and scientists from TAU’s Faculty of Engineering and Sagol School of Neuroscience have developed a newsmartphone-based system that detects changes in patients’ behavioral patterns, and then transmits them to professionals (and/or police? – N.W.) in real time. It has the potential to greatly improve the response time and efficacy of clinical psychiatrists. By facilitating patient observation through smartphones, the technology also affords patients much-needed independence from hospitals, clinicians — and even family members.
Research on the application was presented in March at the Israel Society for Biological Psychiatry’s annual conference. The project won funding from the Israeli Ministry of Economy and was recently chosen as one of four finalist start-up initiatives featured at Israel’s leading Entrepreneurship and Innovation 8200 Accelerator Program. The team is currently in talks with other medical centers in Israel and overseas to expand clinical trials.
Using tools already “in the hand”
“The diagnosis of mental health disease is based only on behavioral patterns,” said Dr. Nevo. “In some cases, a patient is discharged from the hospital into a vacuum, with no idea how to monitor his or her new state of mind. Because most people own smartphones today, we thought, ‘Why not harness the smartphone, a reservoir of daily activities, to monitor behavioral patterns?’
“Bipolar disorder, for example, starts with a manic episode,” said Dr. Nevo. “A patient who usually makes five or ten calls a day might suddenly start making dozens of calls a day. How much they talk, text, how many places they visit, when they go to bed and for how long — these are all indicators of mental health and provide important insights to clinicians who want to catch a disorder before it is full blown.”
Researchers conducted two Helsinki-approved clinical trials with the cooperation and direction of leading psychiatrists from Geha Mental Health Center and Be’er Ya’acov Mental Health Center. In the trials, the application was installed on the smartphones of 20 patients suffering from bipolar, unipolar/depressive, or schizo-affective disorders, as well as on the phones of 20 healthy participants. Over the course of six months,the app acquired data from patients’ phones and sent the information to distant computers, where advanced algorithms analyzed the data to detect changes in patients’ sleep, communication, mobility, and vocal patterns. The researchers further developed a visualization system that displayed the summarized information to psychiatrists, providing them with instant insight into the behavioral trends of their patients.
Preserving patient privacy
According to Dr. Nevo, a patient using the app has full control over who has access to the behavioral patterns recorded and analyzed by it. “We take great care to protect the patient’s privacy,” said Dr. Nevo. “The content of calls and texts is completely ignored and never acquired or recorded, and any identifying parameters of the patient or of his contacts, are irreversibly masked and are obviously not used.”
Psychiatrists in the trials reported that the system has already positively affected their interaction with patients, offering a useful objective “window” into the patient’s daily routine. One patient who was involved in the clinical trial for only a brief period recently suffered a hospitalization. “If I had kept the app on my phone, you would have immediately noticed the unusual number of phone calls I was making, and this hospitalization could have been prevented,” he told his psychiatrist.
“We have a way to go until such a system will be proven effective and adopted by the psychiatric community,” said Dr. Nevo. “However, psychiatrists, as well as U.S. federal policymakers in the field, agree that such tools are necessary to improve psychiatric practice.”
The concluding patient privacy statement is riddled with every falsehood that we already know about how digital data is used by anyone who wishes to gain access.
The communications gadgets that we have purchased already have opened the door to our personal lives. But social engineers know that for the final prison grid to be built they must have full access to our minds. Now that these new tools are coming on the market, the full scope of their applications are being revealed.

